Introduction: Understanding the Severity of Advanced Endometriosis
If you or a loved one has been diagnosed with or suspects end stages of endometriosis, you are likely navigating a storm of questions, fears, and uncertainty. The term itself can sound daunting, even final. But what does it truly mean?
This comprehensive guide is designed to demystify severe endometriosis, specifically focusing on what is clinically known as Stage 4. We will move beyond basic definitions to provide a deep, empathetic, and medically accurate exploration of your condition. Our goal is to empower you with knowledge, clarify your treatment options, and, most importantly, instill a sense of hope and control.
Endometriosis is a complex, chronic condition where tissue similar to the uterine lining grows outside the uterus. When it progresses to its most advanced form, it presents unique challenges. This article will serve as your detailed roadmap, covering everything from the intricate symptoms and the stark reality of infertility to the gold-standard surgical treatments and strategies for reclaiming your quality of life. Let’s begin by breaking down the very definition of this advanced stage.
What Does “End Stages of Endometriosis” Actually Mean?
The phrase “end stages of endometriosis” is not a formal clinical term but a common way to refer to the most severe manifestation of the disease, classified as Stage 4 (Severe) Endometriosis under the system from the American Society for Reproductive Medicine (ASRM).
It is crucial to understand from the outset: “End stage” describes the extent and invasion of the disease, not your life or your hope for recovery. It is a measure of how widespread the endometrial-like tissue has become, not a terminal prognosis.
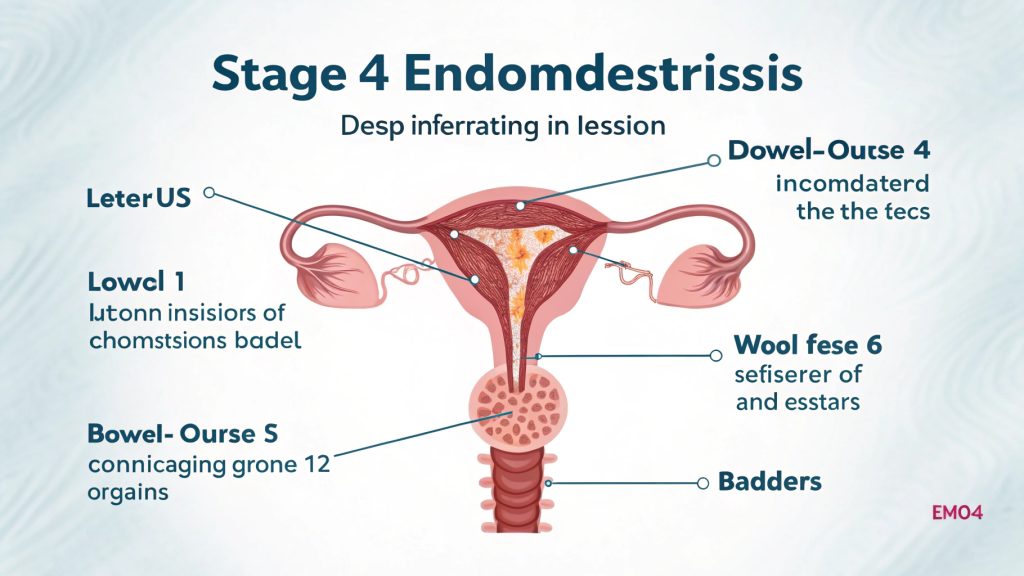
In Stage 4 Endometriosis, the defining characteristics include:
- Deep Infiltrating Endometriosis (DIE): This is a hallmark. Lesions are not superficial; they penetrate deeply—more than 5mm—into the pelvic tissues and organs. This deep invasion is a primary source of the significant pain and organ dysfunction associated with this stage.
- Dense and Widespread Adhesions: The body’s inflammatory response to endometriosis can cause sticky, web-like bands of scar tissue (adhesions) to form. In severe endometriosis, these adhesions are dense and can bind organs together, distorting pelvic anatomy. For example, the ovaries, fallopian tubes, uterus, bowel, and bladder may become fused.
- Large Endometriomas: These are cysts on the ovaries filled with dark, old blood, often referred to as “chocolate cysts.” In Stage 4, these cysts are typically large, often exceeding 3-4 centimeters.
- Multi-Organ Involvement: The disease frequently extends beyond the reproductive organs. It can infiltrate the:
- Gastrointestinal Tract: Bowel, appendix, and rectum.
- Urinary System: Bladder and, in rare cases, the ureters (tubes from kidneys to bladder), potentially causing kidney damage.
- Pelvic Nerves: Such as the sciatic nerve, leading to radiating leg pain (sciatica).
- Cul-de-sac: The space between the uterus and rectum, which may become partially or completely obliterated by disease.
The Staging System: A Deeper Dive into the ASRM Classification

To fully grasp what the end stages of endometriosis entail, it helps to understand the scale. The ASRM staging system (I-IV) is based on a point system evaluated during laparoscopy, considering:
- The Extent of the Implants: Their location, number, and depth (superficial vs. deep).
- The Presence and Severity of Adhesions: How extensive they are and whether they are filmy or dense.
While this system provides a common language for surgeons, a key point of patient advocacy is that the stage does not always correlate perfectly with pain levels. A person with minimal, Stage 1 disease can experience excruciating pain, while someone with widespread Stage 4 might have less apparent symptoms, only to discover the severity during an investigation for infertility. However, deep infiltrating disease is strongly linked to specific types of severe pain.
Unmasking the Symptoms: Beyond “Bad Periods”
The symptoms of End Stages of Endometriosis are often a dramatic and debilitating intensification of the general symptoms of the condition. They extend far beyond the concept of a “bad period.”
Primary Symptoms of Severe Endometriosis:
- Chronic Pelvic Pain: This is no longer just cyclical. The pain can be constant, a dull, heavy ache caused by inflammation, deep lesions, and adhesions pulling on organs.
- Dysmenorrhea (Severe Period Pain): Menstrual cramps are incapacitating, often requiring bed rest and strong pain medication, and not relieved by standard NSAIDs.
- Dyspareunia (Deep Pain During or After Sex): This is a classic sign of deep infiltrating endometriosis (DIE), particularly when lesions are located in the cul-de-sac or uterosacral ligaments. The pain is often described as a “deep, sharp, or tearing” sensation.
- Severe Gastrointestinal Distress: This includes:
- Dysphasia: Painful bowel movements, especially during menstruation.
- Cyclical diarrhea, constipation, or bloating that mirrors Irritable Bowel Syndrome (IBS).
- Rectal bleeding during your period if the bowel is involved.
- Urinary Tract Symptoms: Painful urination (dysuria), frequent urination, or blood in the urine (hematuria) during menstruation if the bladder is affected.
- Profound Fatigue: This is not just tiredness. It is a bone-deep exhaustion that rest does not cure, likely linked to the body’s constant fight against inflammation and chronic pain.
- Infertility: This is one of the most significant consequences of end stages of endometriosis and deserves its own section.
Less Common but Serious Symptoms:
- Sciatic Nerve Pain: Pain radiating down the leg, following the path of the sciatic nerve.
- Shoulder Tip Pain: A rare but telling sign if endometriosis has migrated to the diaphragm, causing referred pain in the shoulder.
- Low Back Pain: Persistent and often cyclical pain in the lower back .
End Stages of Endometriosis and Fertility: Confronting the Reality with Hope
The link between advanced endometriosis and infertility is strong and multi-faceted. For many, the journey to a End Stages of Endometriosis diagnosis begins with the heartbreak of unsuccessful attempts to conceive.
How Does Severe Endometriosis Cause Infertility?
- Anatomical Distortion: Dense adhesions can “freeze” the pelvic anatomy. They can encase the ovaries, preventing the release of an egg, or block and distort the fallopian tubes, making it impossible for the egg and sperm to meet.
- Tubal Damage: The tubes may be scarred or blocked, or their delicate, finger-like fimbriae (which sweep up the egg) may be damaged by adhesions or endometriomas.
- Ovarian Reserve Damage: Large endometriomas and the surgery to remove them can inadvertently damage or remove healthy ovarian tissue, reducing a woman’s egg supply (ovarian reserve).
- Hostile Pelvic Environment: The chronic inflammation associated with end stages of endometriosis can impair sperm function, hinder egg quality, and create a toxic environment that interferes with fertilization and embryo implantation.
The Path to Parenthood: Hope and Options
A diagnosis of Stage 4 endometriosis/ End Stages of Endometriosis does not mean you cannot have children. It means your path may require more planning and medical intervention.
- Excision Surgery: For many, comprehensive excision surgery (discussed in detail below) can improve natural conception chances by restoring normal pelvic anatomy and reducing inflammation. Success depends on the patient’s age and the severity of the tubal damage.
- In Vitro Fertilization (IVF): IVF is often the most successful path. It bypasses many of the barriers posed by endometriosis (like blocked tubes or hostile mucus) by fertilizing the egg in a lab and transferring the embryo directly into the uterus. Prior excision surgery can significantly improve IVF success rates by creating a healthier environment for implantation.
A consultation with both a qualified endometriosis excision specialist and a Reproductive Endocrinologist (fertility specialist) is crucial to create a personalized plan.
The Gold Standard: Diagnosis and Treatment for Advanced Endometriosis
Navigating treatment for end stages of endometriosis requires a sophisticated approach. The cornerstone of effective management is an accurate diagnosis and skilled, radical surgery.
Diagnosis: The Role of Advanced Imaging
While a definitive diagnosis still requires laparoscopy, skilled radiologists using advanced imaging can strongly suspect Stage 4 endometriosis or End Stages of Endometriosis.
- Transvaginal Ultrasound: When performed by a specialist trained in detecting deep infiltrating endometriosis, this can identify endometriomas, adhesions, and bowel and bladder involvement.
- Magnetic Resonance Imaging (MRI): An MRI with pelvic protocol can provide a detailed “map” of the disease, confirming deep infiltrating lesions in the bowel, bladder, and rectovaginal septum. This is invaluable for pre-surgical planning.
Excision Surgery: The Gold Standard Treatment
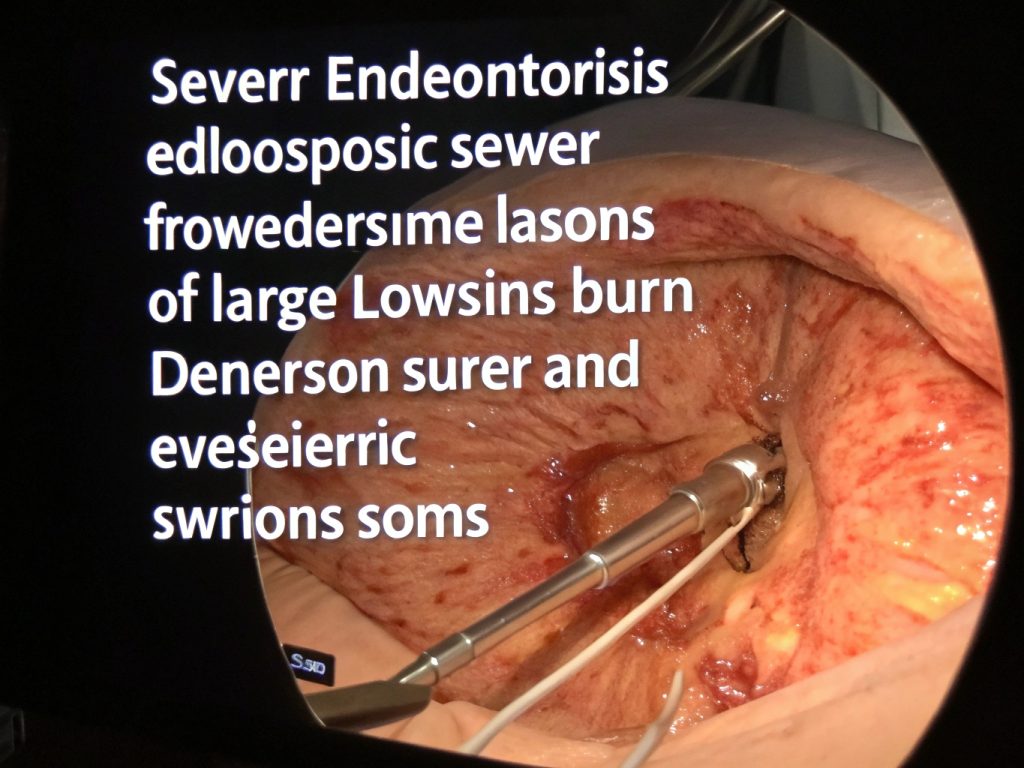
For the end stages of endometriosis, excision surgery is widely considered the most effective long-term treatment.
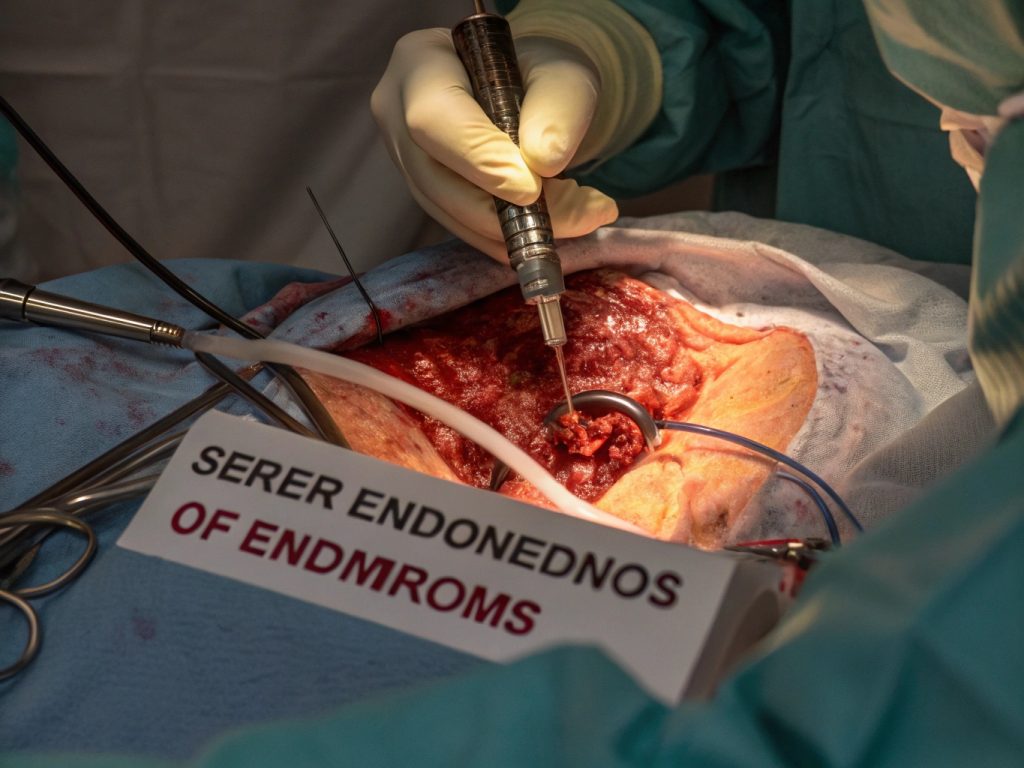
What is Excision Surgery?
It is a meticulous surgical technique where a skilled surgeon identifies and cuts out (excises) each lesion of endometriosis at its root, preserving as much healthy tissue as possible. This is in contrast to ablation (burning the surface), which is less effective for deep disease.
The Goal of Excision for End Stages of Endometriosis:
- Restore Normal Anatomy: Carefully dissect and remove adhesions to free organs.
- Achieve Complete Cytoreduction: Remove every visible implant of endometriosis.
- Preserve Organ Function: This is critical, especially when the disease is on the bowel, bladder, or ureters. This may require a multi-disciplinary surgical team, including a endometriosis specialist and a colorectal or urologic surgeon.
The expertise of the surgeon is the single most important factor in the success of this surgery. Finding a surgeon who specializes in this technique is non-negotiable for achieving the best outcomes.
Complementary and Adjunctive Therapies
Surgery is the cornerstone, but a multi-modal approach is essential for managing a chronic condition.
- Hormonal Suppression (Post-Surgery): After excision, medications like GnRH agonists (e.g., Lupron), continuous birth control, or progestins may be used to suppress any microscopic disease and manage pain. They are a tool for management, not a cure for existing deep disease.
- Pain Management: A comprehensive plan may include prescription NSAIDs, nerve pain medications (like Gabapentin), and sometimes referral to a pain management specialist.
- Pelvic Floor Physical Therapy: This is a critical, often overlooked component. Chronic pain and inflammation cause pelvic floor muscles to become incredibly tight and painful (hypertonic). A specialized physical therapist can release these trigger points, break down scar tissue, and retrain the muscles, providing significant pain relief.
- Diet and Nutrition: While no specific “endometriosis diet” is proven to cure the disease, an anti-inflammatory diet (rich in omega-3s, low in red meat and processed foods) can help some individuals manage systemic inflammation and symptoms.
- Integrative Approaches: Acupuncture, mindfulness, and cognitive-behavioral therapy (CBT) can be powerful tools for managing the stress, anxiety, and pain perception associated with chronic illness.
Living a Full Life with Severe Endometriosis: A Conclusion of Empowerment
Receiving a diagnosis of end stages of endometriosis can feel like an ending. But we want to reframe it as a beginning—the start of a path toward definitive treatment and renewed quality of life.
The journey is undeniably challenging, but you are not powerless. The key takeaways are:
- “End Stage” is a Description, Not a Destiny: It defines the extent of the disease, not your future.
- Expert Care is Paramount: Your most critical step is to find an endometriosis excision specialist with proven experience in handling complex, Stage 4 cases, including multi-organ involvement.
- A Multi-Faceted Approach Wins: Combine expert surgery with physical therapy, nutritional support, and mental health care for the best results.
- Hope is a Valid Emotion: With proper treatment, most women experience a dramatic reduction in pain and a significant improvement in their quality of life. For those facing infertility, medical science offers powerful pathways to parenthood.
Your pain is real. Your struggle is valid. And with the right knowledge and the right team, your future can be one of health, vitality, and hope.
Frequently Asked Questions (FAQ)
Q1: Is Stage 4 endometriosis cancer?
A: No, endometriosis is a benign (non-cancerous) condition. However, its invasive and spreading nature has led some to call it “cancer-like,” and it does carry a very slightly increased risk of certain ovarian cancers, which is why proper management is crucial.
Q2: Can a hysterectomy cure my Stage 4 endometriosis?
A: Not necessarily. A hysterectomy (removal of the uterus) may help if your pain is primarily centered in the uterus, but it does not remove endometriosis lesions that are already on your bowel, bladder, pelvic walls, or elsewhere. The gold standard remains excision of all endometriosis lesions, regardless of whether a hysterectomy is performed.
Q3: What’s the difference between ablation and excision surgery?
A: Ablation uses heat or laser to destroy the surface of an endometriosis lesion. It is like mowing a weed. Excision surgery involves cutting out the entire lesion, including its root. For deep infiltrating endometriosis, excision is the only effective method to fully remove the disease.
Q4: How do I find a qualified endometriosis specialist?
A: Look for a surgeon who:
- Specializes in Advanced Laparoscopic Surgery and specifically mentions excision as their primary technique.
- Performs a high volume of endometriosis surgeries regularly.
- Works as part of a multi-disciplinary team for complex cases.
- Is affiliated with reputable hospitals or specialized endometriosis centers.
- Has positive, verified patient testimonials.

Pingback: Effective Hormone Replacement Therapy for Women's Health-25